Requirements:
- ≥ 1000 covered lives
- Self-funded
- Access to all claims data (previous 12 months and throughout the program)
- Minimum 1-year commitment
- On-site/near-site clinics
- Coverage of FDA-approved anti-obesity pharmaceutical agents (for employees that meet qualifications, preferably only when prescribed by clinicians with advanced training in Obesity Medicine in conjunction with an intensive lifestyle intervention)
Recommended:
- inBody body composition machine in the clinic(s)
- Health coach access (can be provided via an electronic platform for an additional fee)
Pre-Implementation:
- Mutual agreement re: program goals and metrics to measure
- Clinical: BMI (optional body fat %), A1C, blood pressure, TG, HDL, Fib-4 index
- Financial: Overall claims, claims per person (w/ and w/out obesity)
- Absenteeism, workman’s compensation claims, short- and long-term disability claims
- Systematic linking of multiple sources of data, ensuring the confidentiality of employee information
- healthcare claims data from the prior year & 12 months during the program
- workman’s compensation, short- and long-term disability, and absenteeism data from the prior year and 12 months during the program
- Training of on-site/near-site clinical staff:
- All providers (MDs/DOs/NPs/PAs) and health coach (if applicable): 8 hours in-person
- Ancillary staff (MAs, CNAs, LPNs, RNs): 1-hour in-person
- Integration into EHR system:
- WellMi will work with super-user to create/adapt templates and upload pertinent handouts
- List of demographic characteristics
- Multiple opportunities and methods for all employees to learn about and participate in the program’s activities
- Agreement about optional tier 2 (personalized health coaching) available on the app (employee fully responsible for the additional monthly subscription fee vs partially/fully subsidized by employer)
- Senior leadership support, identification of a workplace coordinator
Ongoing:
- Clinical staff have access to the WellMi team via email for questions/concerns
- WellMi team will offer clinical staff weekly town hall meetings via zoom
- All employees (≥ 18 years of age) will have free access to the basic WellMi electronic platform with the option to purchase a tier 2 monthly subscription ($40/month for personalized coaching)
- Data analyzed & reported quarterly
After 12 months:
- Full data analysis and report of savings
- Renewal option
*For obvious privacy reasons, individual-level measures will be collected anonymously and only reported in the aggregate. The company will be provided with data relative to the previous year’s costs as well as data contrasting program participants with non-participants
Estimated Costs:
YEAR 1:
Tier 1 electronic platform: 15,000 employees x $5 PMPM: $900,000
Training & ongoing support of clinical staff (6 clinicians x $5K/year): $30,000
Set up/roll-out/integration/data-analytics x $2 PMPM: $360,000
______________________
$1,290,000
(waived for pilot study)
YEAR 2:
Tier 1 electronic platform: 15,000 employees x $5 PMPM: $900,000
Training & ongoing support of clinical staff (6 clinicians x $5K/year): $30,000
Set up/roll-out/integration/data-analytics x $1 PMPM: $180,000
_______________________
$1,110,000
KPIs:
HEALTHCARE COSTS:
Because of the unknown at-risk population and the potential for discovery of previously unidentified diagnoses requiring treatment and associated cost implications, the effect of a health promotion program may not be reflected in reduced health care expenditures immediately. In fact, it is possible that in the short term, utilization of services will increase, resulting in higher health care expenditures. We will attempt to separate new diagnoses from preexisting, previously unrecognized diagnoses, but given the limitations in the medical coding system, in some cases, this data may be difficult to separate. Regardless of this initial data, long-term data is solid, showing an increase in preventive services will reduce or delay the development of various diseases, which will, in turn, reduce future healthcare expenditures. There exist several validated studies demonstrating the cost-effectiveness relative to improvements in certain parameters and in addition to overall costs, these specific parameters will be measured:
HEALTH OUTCOMES
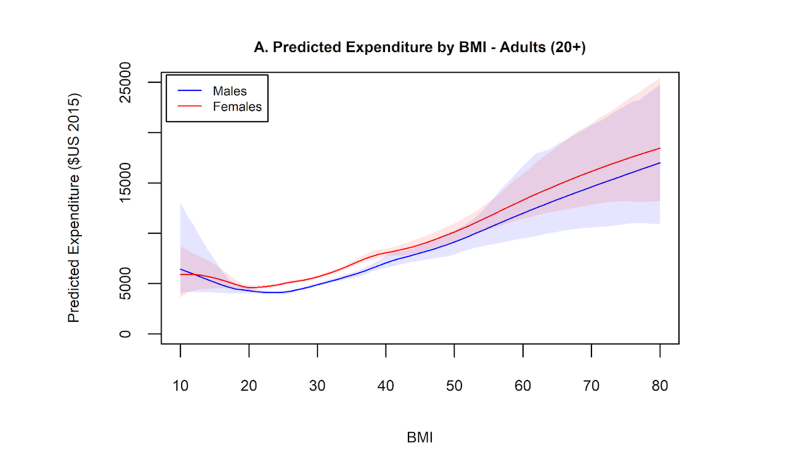
BMI: BMI is a ratio of height/weight. Although it isn’t completely accurate in estimating adiposity (the presence of excess fat mass), it is accurate more often than not. In the absence of quantitative body fat percentage measurements, it is the most accurate way we have of determining pre-obesity and obesity. There exists a linear relationship between BMI and health care costs. Above a BMI threshold of 30, we know that each one-unit BMI increase is associated with an additional cost of $253 per person.
Glycated Hemoglobin (Hgb A1C): is an estimate of the average blood sugar for the previous three months. ≤ 5.6 is normal, 5.7-6.4 denotes prediabetes and ≥ 6.5 is considered diabetes. Numerous studies conclude that keeping A1C in the desired range can help reduce complications of diabetes, such as high blood pressure, cardiovascular disease (which can result in heart attack and stroke), vascular insufficiency (which can result in amputation), retinopathy (which can result in blindness), chronic kidney disease (which can result in dialysis and need for transplantation), nerve damage (which can result in decreased mobility and disability). Data has shown that for every 1% increase in Hgb A1C, health care costs rise at least 7% over the subsequent 3 years. For patients with HbA1c ≥7%, a 1% reduction is associated with a 1.7% reduction in all-cause total healthcare costs and a 6.9% reduction in diabetes-related healthcare costs of $545 and $555, respectively.
Triglycerides: Triglycerides are a type of fat (lipid) found in the bloodstream and fasting levels should be below 150 mg/dL in adults. Studies have consistently linked high triglyceride levels with heart disease, heart attacks, and stroke, especially in people with low levels of “good” HDL cholesterol and in those with type 2 diabetes. Aside from patients with familial hypercholesterolemia (a gene mutation), triglyceride levels are a good reflection of overall health, reflecting things such as dietary composition, exercise, stress, sleep, and alcohol/tobacco use. We have data linking high triglyceride levels with increased health care utilization and costs by 33-38% independent of resource-intensive conditions such as cardiovascular disease, heart failure, hypertension, and diabetes.
Blood Pressure: Hypertension is defined as a systolic blood pressure ≥ 140 mm Hg or a diastolic blood pressure ≥ 90 mm Hg. Chronic hypertension can cause heart disease, stroke, chronic kidney disease (CKD), and blindness. Hypertension is easy to diagnose and is inexpensive to treat with medications, however, mild to moderate hypertension is rarely symptomatic and medication adherence is often poor. 75% of adults with a diagnosis of hypertension do not meet the criteria for being well-controlled. High treatment costs are typically related to disease complications due to poor control and are cumulative and progressive. The combination of obesity and hypertension confers exponential risk in terms of long-term severe complications such as cardiovascular disease. For individuals already afflicted by the obesity-hypertension phenotype, interventions must aggressively focus on weight loss and blood pressure control.
HDL: Although HDL is often referred to as “good” cholesterol, its presence in the bloodstream is actually quite complex. Just as a high HDL level is a marker for overall health, a low HDL level is a marker for suboptimal health. The optimal level of HDL cholesterol for both men and women is ≥ 60 mg/dL and a level below 40 mg/dL in men and below 50 mg/dL in women is considered risky for the development of cardiovascular disease. Smoking, inactivity, diabetes, excess weight, poor eating habits, and chronic stress all lower HDL cholesterol. As already noted, it takes years for abnormal blood cholesterol levels to lead to coronary heart disease or heart attack, but early intervention is essential for the prevention of cardiovascular disease.
FIB-4 index: The FIB-4 index is a screening test for NAFLD (non-alcoholic fatty liver disease). As of 2022, approximately 25% of Americans have NAFLD. Among these individuals, 12-14% develop nonalcoholic steatohepatitis (NASH), which can progress to fibrosis, cirrhosis, portal hypertension, decompensated liver disease, and hepatocellular carcinoma. NASH currently follows hepatitis C as the second most common reason for liver transplantation in the US. Recent guidelines issued by the AACE issued guidelines to diagnose and treat all patients at high risk for NAFLD, including those with obesity, prediabetes, T2DM, and/or ≥ 2 other features of metabolic syndrome (hypertension, high triglycerides, and/or low HDL cholesterol). The FIB-4 score is calculated using the patient’s age, AST/ALT levels (liver function tests), and platelet count. Dietary modifications and physical activity that improves body composition and cardiometabolic health are the only treatments currently available for patients with NAFLD. For patients with overweight or obesity, the recommendation is to lose at least 5% and preferably ≥10% of their body weight, as more weight loss is associated with greater cardiometabolic benefit and reductions in NASH or fibrosis.
HEALTHCARE USE:
Analysis of the utilization of various types of healthcare services (outpatient care, inpatient care, emergency room visits, pharmaceuticals, radiology services, and physical therapy visits) will be measured. The majority of the increased healthcare costs related to obesity come from a 90% increase in the cost of inpatient services, a 38% increase in the cost of non-inpatient services, and an 82% increase in the cost of prescription drugs. Although treating obesity increases outpatient visits, the increase in costs for these services is outweighed by the decrease in inpatient visits and ER visits – two service lines that are significantly more expensive.
INDIRECT COSTS: (ABSENTEEISM, PRESENTEEISM. WORK-RELATED DISABILITY CLAIMS, AND WORKER’S COMPENSATION): While direct medical expenditures are the most manifest costs of illnesses caused by obesity, they are by no means the only costs. Obesity-related illnesses take their toll in lost productivity. Healthier employees are less likely to call in sick. Studies have repeatedly found that employees with obesity are 25% to 100% more likely to be absent from work compared with employees of normal weight. When physically present at work, employees with obesity demonstrate a significantly higher rate of presenteeism, due to higher rates of emotional exhaustion, psychological complaints, and lower quality of life.
Employees with obesity have higher costs in the areas of disability and workers’ compensation. Multiple studies have demonstrated that employees with obesity have 239%-700% more workers’ compensation days and 143%-550% more costs than employees with normal weight. MSK issues prompt a majority of worker’s compensation claims and account for a disproportionate amount of outpatient, hospital, and emergency room visits. MSK issues are much more common in people with excess weight and are typically improved, if not resolved, with decreases in weight.
If the company already has measures in place to evaluate and calculate productivity, these metrics will continue to be used throughout the program. If not, sick day use is a crude evaluation of worker productivity and will be used. Working with company representatives, we will attempt to determine the costs of worker absenteeism including costs of replacement workers, costs in training replacement workers, and loss and delay in productivity. Time spent during working hours participating in obesity-related worksite programs will be taken into consideration.
References:
- Mercer US. Health Benefit Plans & Survey 2022. https://www.mercer.us/what-we-do/health-and-benefits/strategy-and-transformation/mercer-national-survey-benefit-trends.html. Accessed September 2, 2022
- Centers for Disease Control and Prevention. Health Care Costs / Obesity Evaluation Measures. https://www.cdc.gov/workplacehealthpromotion/health-strategies/obesity/evaluation-measures/health-care-cost.html, accessed September 2, 2022.
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, Dietz W. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012 Jun;42(6):563-70. doi: 10.1016/j.amepre.2011.10.026.
- American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care 2018;41(5):917–928. https://doi.org/10.2337/dci18-0007
- Centers for Disease Control and Prevention. Cost-Effectiveness of Diabetes Interventions. https://www.cdc.gov/chronicdisease/programs-impact/pop/diabetes.htm, accessed September 2, 2022.
- Centers for Disease Control and Prevention. Healthcare Cost Data. https://www.cdc.gov/workplacehealthpromotion/model/healthcare-cost-data/index., accessed September 2, 2022.
- White J, Hartley SK, Musich S, Hawkins K, Ozmminkowski RJ. A More Generalizable Method to Evaluate the Association Between Commonly Reported Health Risks and Health Care Expenditures Among Employers of All Sizes. J Occup and Environ Med 2013;55(10):1179-1185. DOI:10.1097/JOM.0b013e31829b2833
- Ward ZJ, Bleich SN, Long MW, Gortmaker SL (2021) Association of body mass index with health care expenditures in the United States by age and sex. PLOS ONE 16(3): e0247307. https://doi.org/10.1371/journal.pone.0247307
- Truls O, Stroo M, Eisenstein EL, Peterson B, Dement J (2014) Is Overweight and Class I Obesity Associated with Increased Health Claims Costs? Obesity (2014) 22, 1179–1186. doi:10.1002/oby.20669
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013 Apr;36(4):1033-46. doi: 10.2337/dc12-2625. Epub 2013 Mar 6. PMID: 23468086; PMCID: PMC3609540
- Lage MJ, Boye KS. The relationship between HbA1c reduction and healthcare costs among patients with type 2 diabetes: evidence from a U.S. claims database. Curr Med Res Opin. 2020 Sep;36(9):1441-1447. doi: 10.1080/03007995.2020.1787971. Epub 2020 Jul 17. PMID: 32643451.
- Gilmer TP, O’Connor PJ, Manning WG, Rush WA. The cost to health plans of poor glycemic control. Diabetes Care. 1997;20(12):1847-53. Crossref, Medline, Google Scholar
- Arena R, Daugherty J, Bond S, Lavie CJ, Phillips S, Borghi-Silva A. The combination of obesity and hypertension: a highly unfavorable phenotype requiring attention. Curr Opin Cardiol. 2016 Jul;31(4):394-401. doi: 10.1097/HCO.0000000000000294. PMID: 27070650
- Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017 Aug;122:1-7. doi: 10.1016/j.phrs.2017.05.013. Epub 2017 May 19. PMID: 28532816.
- Nichols GA, Phillip S, Reynolds K, Granowitz CB, O’Keeffe-Rosetti M, Fazio S. Comparison of Medical Care Utilization and Costs Among Patients With Statin-Controlled Low-Density Lipoprotein Cholesterol With Versus Without Hypertriglyceridemia. Am J Cardiol 2018;Jul 5:2018
- Nichols GA, Arondekar B, Garrison Jr. LP. Patient Characteristics and Medical Care Costs Associated With Hypertriglyceridemia. Am J Cardiol 2011; Jan 15: 107, 2 (225-229)
- Hay, Joel & Sterling, Kimberly. (2005). Cost Effectiveness of Treating Low HDL-Cholesterol in the Primary Prevention of Coronary Heart Disease. PharmacoEconomics. 23. 133-41. 10.2165/00019053-200523020-00005.
- Cusi K, Isaacs S, Barb D, et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocrine Practice. 2022;28(5):528-562.
- Kanwal F, Shubrook JH, Younossi Z, et al. Preparing for the NASH Epidemic: A Call to Action. Diabetes Care. 2021;44(9):2162-2172.
- DiBonaventura M, Le Lay A, Kumar M, Hammer M, Wolden ML. The Association Between Body Mass Index and Health and Economic Outcomes in the United States. J Occup and Environ Med 2015;57(10):1047-1054. DOI:10.1097/JOM.0000000000000539
- Kleinman N, Abouzaid S, Andersen L, Wang Z, Powers A. Cohort analysis assessing medical and nonmedical cost associated with obesity in the workplace. J Occup Environ Med. 2014 Feb;56(2):161-70. doi: 10.1097/JOM.0000000000000099. PMID: 24451611.
